According to the Environmental Protection Agency, approximately 100 million dental x-rays are done each year in the United States. These x–rays provide your dentist with a vital tool that shows the condition of your teeth including roots, jaw placements, and the overall composition of your facial bones. X-ray machines only produce radiation during operation and the amount of radiation used is small.
Sealants are a thin, plastic coating that are painted on the chewing surfaces of teeth -- usually the back teeth (the premolars, and molars) – to prevent tooth decay. The painted on liquid sealant quickly bonds into the depressions and grooves of the teeth forming a protective shield over the enamel of each tooth. Typically, children are most cavity prone from ages 6 to 14 so the American Dental Association (ADA) recommends they should get sealants on the permanent molars and premolars as these teeth come in. Dental sealants can protect their teeth from decay for up to 10 years.
FDA rules mercury amalgam fillings safe. The U.S. Food and Drug Administration's long-awaited final regulation on the use of mercury amalgam for dental fillings deems the material safe, while at the same time moving the material from the Class I (low risk) medical-device category to Class II (moderate risk). This allows for tighter control over its manufacture and use. Mercury amalgam, or 'silver,' fillings have been used for decades to repair cavities. It's the cheapest filling material available, and the American Dental Association (which supports the new regulation) has long warned that restricting its use would deprive dentists of an important tool and likely move needed dental work beyond the reach of low-income patients. But many people have raised concerns about the potential for mercury to 'leak' from fillings into the body and cause neurological damage or diseases such as multiple sclerosis. An FDA press release announcing the decision reports: 'While elemental mercury has been associated with adverse health effects at high exposures, the levels released by dental amalgam fillings are not high enough to cause harm in patients.' Still, the agency suggests that amalgam package labels feature a warning to patients about the risk of mercury allergy, a reminder to dental professionals about the risk of working with mercury amalgam without proper ventilation, and 'a statement discussing the scientific evidence on the benefits and risk of dental amalgam, including the risks of inhaled mercury vapor. The statement will help dentists and patients make informed decisions about the use of dental amalgam,' according to the press release.
Each of these options differ with regard to cost, durability, 'chair time' necessary to complete the procedure, stain resistant qualities, and best cosmetic approach to resolving a specific problem. Talk to your dentist to see if one is right for you.
Amalgam (silver filling) is the most thoroughly researched and tested restorative material among all those in use. It is durable, easy to use, highly resistant to wear and relatively inexpensive in comparison to other materials. For those reasons, it remains a valued treatment option for dentists and their patients.
While questions have arisen about the safety of dental amalgam relating to its mercury content, the major U.S. and international scientific and health bodies, including the National Institute of Health, the U.S. Public Health Service, the Centers for Disease Control and Prevention, the Food and Drug Administration and the World Health Organization, among others have been satisfied that dental amalgam is a safe, reliable and effective restorative material.
Because amalgam fillings can withstand very high chewing loads, they are particularly useful for restoring molars in the back of the mouth where chewing load is greatest. They are also useful in areas where a cavity preparation is difficult to keep dry during the filling replacement, such as in deep fillings below the gum line. Amalgam fillings, like other filling materials, are considered biocompatible—they are well tolerated by patients with only rare occurrences of allergic response.
Disadvantages of amalgam include possible short-term sensitivity to hot or cold after the filling is placed. The silver-colored filling is not as natural looking as one that is tooth-colored, especially when the restoration is near the front of the mouth, and shows when the patient laughs or speaks. And to prepare the tooth, the dentist may need to remove more tooth structure to accommodate an amalgam filling than for other types of fillings.
According to the American Academy of Pediatric Dentistry – your child should visit a pediatric dentist when the first tooth comes in, usually between 6 and 12 months of age. This visit will establish a dental home for your child. Early examination and preventive care will protect your child’s smile now and in the future.
A child's primary teeth, sometimes called 'baby teeth,' are as important as the permanent adult teeth. Primary teeth typically begin to appear when a baby is between age six months and one year and help children chew and speak. They also hold space in the jaws for permanent teeth that are developing under the gums. The ADA recommends that a dentist examine a child within six months of the eruption of the first tooth and no later than the first birthday. A dental visit at an early age is a 'well baby checkup' for the teeth. Besides checking for tooth decay and other problems, the dentist can demonstrate how to clean the child's teeth properly and how to evaluate any adverse habits such as thumbsucking.
Have your child rinse their mouth with warm water to clean it out. Gently use dental floss or an interdental cleaner to ensure that there is no food or other debris caught between the teeth. In addition, the ADA recommends to place a cold compress on the face if it is swollen. If the pain persists, contact your dentist.
The sooner the better! Starting at birth, clean your child’s gums with a soft infant toothbrush or cloth and water. Then, according to the American Adacemy of Pediatric Dentistry,as soon as the teeth begin to appear, start brushing twice daily using fluoridated toothpaste and a soft, age-appropriate sized toothbrush. Use a 'smear' of toothpaste to brush the teeth of a child less than 2 years of age. For the 2-5 year old, dispense a 'pea-size' amount of toothpaste and perform or assist your child’s toothbrushing. Remember that young children do not have the ability to brush their teeth effectively. Children should spit out and not swallow excess toothpaste after brushing.
Fluoride, a naturally occurring mineral, is often added to drinking water and is commonly found in toothpaste. Research has shown that the rate of cavities decreases in areas where fluoride is added to the water supply. Health authorities, such as The American Dental Association and The World Health Organization, both advocate the addition of fluoride to drinking water, and recommend you use toothpaste that contains fluoride, if age appropriate.
If you do not have fluoride in your water, fluoride is also available in:
Speak with your dentist if you are concerned whether or not you are receiving enough, or too much fluoride daily. Fluoride treatments are also given at your dental office after a cleaning appointment every six months to one year.
Many types of floss are available, either from your dentist or a local retailer. Choose one that will meet your needs. For example, some people have difficulty with floss snagging and breaking because their teeth are in tight contact. There is floss designed for that purpose.
If you have limited dexterity, try using a flossing aid designed to eliminate the need to use both hands. You can discuss your needs with your dentist and get a recommendation.
Look for the ADA Seal of Acceptance on any products you use as an assurance that they have been evaluated for safety and effectiveness. These products currently include dental floss, a wooden plaque remover, and a water flosser.1
Before brushing your teeth, take approximately 18 inches of floss and wind each end around your middle fingers. Grasp 1 to 2 inches of the floss with your index (pointer) finger and thumb.
Gently glide the floss in between the teeth in a sawing motion. Use care not to snap the floss between the teeth as this may cause trauma to the tissue or the tooth itself.
Angle the floss so it hugs the tooth in a “c” shape. Gently slide the floss up and down the surface of the tooth making sure it goes slightly below the gum line.
When complete, angle the floss to hug the tooth in the opposite direction and repeat this step.
Continue flossing all of the upper and lower teeth. Try working in a clockwise direction, beginning with your upper molars on your left side and then ending with your lower molars on your left side. As you move on to each set teeth, unwind the floss from your fingers, and rewind it so there is a clean section of floss to use.
When you have completed flossing, toss the used floss and don't save it to reuse. If you use it again, you reintroduce bacteria and debris that you just worked so hard to remove.
When you have finished flossing, follow with brushing and rinse with either water or mouthwash. You don't necessarily have to brush your teeth after flossing, so don't skip flossing if you don't have a toothbrush and sink handy.
The American Dental Association doesn't take a stand on whether flossing before or after brushing is preferable, and there aren't good studies that say one way is better than the other. What matters is that you clean between your teeth well every day and that you brush your teeth twice a day.1
Floss or use another method to clean between your teeth at least once a day and make it part of your routine. If you don't have time for flossing in the morning, always floss in the evening before your final brush of the day.
Wet your toothbrush with water and apply a thin strip of toothpaste. If you've ever stood in the toothpaste aisle at the store, you can attest to the innumerable types of toothpaste that are available. It all depends on your own preferences, but try to use one that contains fluoride, which protects the teeth against cavities and prevents tooth decay.
Start with your upper molars, or your back teeth, on one side of your mouth and work in a clockwise direction. Point the bristles toward the gum line at a 45-degree angle. Brush using short, circular motions for approximately 20 seconds.
After 20 seconds, roll the brush head away from the gum line so the bristles sweep the surface of the tooth, removing plaque and food particles in the process.
Continue working in a clockwise direction, finishing up with the lower molars on the other side of your mouth.
Repeat steps two and three for the inside surfaces of the upper and lower molars.
Brush the lingual, or back surface of the upper front teeth by using the tip of the toothbrush head. Direct the bristles toward the gum line and use a flicking motion down the surface of the tooth. Repeat this two or three times for a more thorough clean.
Point the bristles of the tip of the toothbrush toward the gum line and flick the bristles up and away from the gum line in a sweeping motion. Repeat this step two or three more times.
Brush the top, biting surfaces of the upper and lower premolars and molars using a circular motion.
Teeth aren't the only things in your mouth that need to be cleaned. Your tongue, the roof of your mouth and the insides of your cheeks can also hold onto food particles, plaque, and bacteria that make your breath smell. Just like your teeth, they deserve a good cleaning. With a gentle, circular motion, thoroughly brush your tongue, the insides of your cheeks and the roof of your mouth.
Mouth health is essential to general health and well being at every stage of life. A healthy mouth enables not only nutrition of the physical body, but also enhances social interaction and promotes self-esteem and feelings of well-being.
Like many areas of the body, your mouth is filled with and generally coping with bacteria; most of them harmless. To be more accurate, the mouth hosts approximately six billion microbes representing 300 to 500 species. Normally the body's natural defenses and good oral health care, such as daily brushing and flossing, can keep these bacteria under control. However, without proper oral hygiene, bacteria can reach levels that might lead to oral infections, such as tooth decay and gum disease.
In addition, certain systemic conditions, diseases and medications — such as decongestants, antihistamines, painkillers and diuretics — can reduce saliva flow. Saliva washes away food and neutralizes acids produced by bacteria in the mouth, helping to protect you from microbial invasion or bacterial overgrowth that might lead to teeth and gum diseases.
The mouth, besides its well known functions, serves as a “window” to the rest of the body, providing signals of general health disorders. For example, aphthous ulcers are occasionally a manifestation of Coeliac disease or Crohn’s disease, pale and bleeding gums can be a marker for blood disorders, bone loss in the lower jaw can be an early indicator of skeletal osteoporosis, mouth lesions may be the first signs of HIV infection, and changes in tooth appearance can indicate bulimia or anorexia.
For decades, physicians and dentists have paid close attention to their own respective fields. Years ago, a physician who suspected heart disease would probably not refer the patient to a gum specialist. The same went for diabetes, pregnancy, or just about any other medical condition. However, recent findings have strongly suggested that oral health may be indicative of systemic health. Currently, this gap between medical and dental practices is quickly closing, due to significant findings supporting the association between periodontal disease (advanced gum disease) and systemic conditions such as cardiovascular disease, type 2 diabetes mellitus, adverse pregnancy outcomes, osteoporosis and other systemic conditions.
Periodontitis, one of the most common oral diseases of humans, is an infectious condition that results in the inflammatory destruction of gum ligaments and the bone surrounding the teeth. As a result of the extensive microbial plaques (deposits) associated with periodontal infections, the chronic nature of these diseases, and the exaggerated local and systemic body response to microbial assault, it is reasonable to hypothesize that these infections may influence overall health and the course of some major systemic diseases affecting the general population, our beloved ones and even ourselves.
Does any one of you remember times were we heard about grandparents or relatives taking all their teeth out and later feeling healthy and energetic? It is not the act of pulling teeth per se that provided the cure. In fact, it was the elimination of all that was attached to the teeth that provided the cure. Science now proves that the bacteria attached to the teeth and associated gum tissues and/or their by products were in fact traveling from the mouth and adversely affecting a remote organ.
Today, physicians should be taking a more holistic approach to their patients’ overall health management. Specialized gum treatment should be an integral part of the medical treatment of many systemic diseases. Studies show that people with serious gum disease were about 40% more likely to have a chronic medical condition on top of it.
The Gateway to Your Body
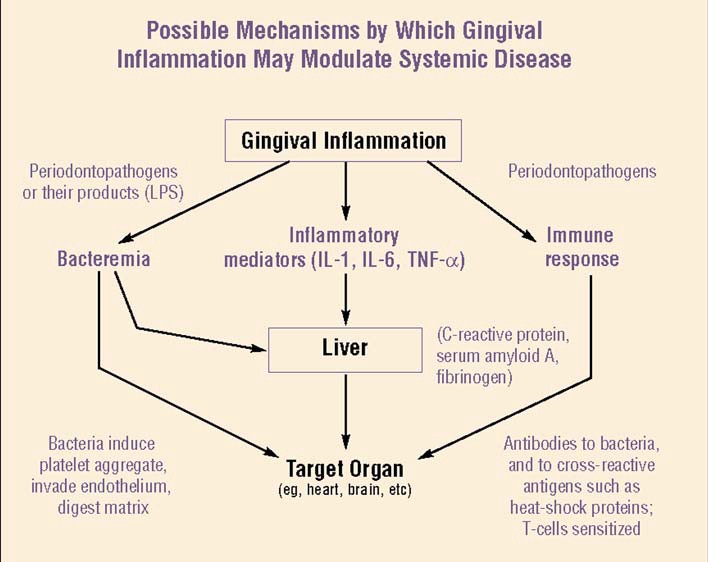
To understand how the mouth can affect the body, it helps to understand what can go wrong in the first place. Bacteria that builds up on teeth, make gums susceptible to infection. The immune system moves in to attack the infection and the gums become inflamed. The inflammation continues unless the infection is brought under control by professional dental care usually by a periodontist (gum therapy specialist).
Over time, without professional dental and gum care, inflammation and the chemicals it releases, eat away the gums and bone structure that hold teeth in place. The result is advanced severe gum disease, known as periodontitis. Inflammation can accordingly cause problems in the rest of the body.
Organ Systems and Conditions Possibly Influenced by Periodontal Infection
Your oral health might affect, be affected by, or contribute to various diseases and conditions, including:
Periodontal (Advanced Gum Disease) and Cardio-vascular Diseases
Oral Health, Heart Disease and Brain Strokes
Cardiovascular disease (CVD) is a common cause of death, accounting for a worldwide 29% of deaths. Millions of people have been diagnosed with different forms forms of CVD, which include high blood pressure, coronary heart disease (myocardial infarction –i.e. heart attacks and angina pectoris), peripheral arterial disease, and stroke, with atherosclerosis as the principal cause of all CVDs. Atherosclerosis refers to the buildup of fats, cholesterol and other substances in and on your artery walls (plaques), which can restrict blood flow. These plaques can burst, triggering a blood clot that can travel through the blood stream and cause a heart attack or brain stroke. Atherosclerosis according to studies is thus responsible for 50% of all mortality in the United States, Europe, and Japan.
After adjustment of other risk factors, studies indicate that severe gum disease is associated with a 25% to 90% increase in risk for CVD . Though the evidence is not yet clear-cut in nature and reasons are not fully understood, it’s clear that gum disease and heart disease often go hand in hand.
Periodontal diseases might affect heart disease through the mechanism of oral bacteria, bacterial toxins (poisonous bacterial by products), and induced inflammatory mediators entering the blood stream and contributing to chronic, systemic vascular challenge, directly resulting in platelet aggregation (accumulation and clustering), adhesion, and vasculitis (inflammation of the vessels), with the subsequent cholesterol deposition, thromboembolic events, and atheroma (clot) formation.
Another possibility is that the inflammation caused by periodontal disease induces inflammatory cell infiltration into major vessels, vascular smooth muscle proliferation (increased growth), vascular fatty degeneration, and increasing plaque build-up, which contribute to swelling and thickening of the arteries. These events may lead to atherosclerosis and atheroma (clot) formation, and result in obstruction of normal blood flow, restricting the amount of nutrients and oxygen required for the heart to function properly, and eventually increase the risk of heart attacks.
Whatever mechanisms are involved, it is evident that periodontitis may affect the host’s susceptibility to systemic disease through subgingival (under the gum) plaque biofilms acting as reservoirs of bacteria and creating transient bacteremia, through release of microbial toxins and through a reservoir of inflammatory mediators. In parallel, all these factors are capable of predisposing the host to vascular changes or disorders.
Collectively speaking, "The theory is that inflammation in the mouth causes inflammation in the blood vessels,". This can increase the risk for heart attack in a number of ways. Inflamed blood vessels allow less blood to travel between the heart and the rest of the body, raising blood pressure. "There’s also a greater risk that fatty plaque will break off the wall of a blood vessel and travel to the heart or the brain, causing a heart attack or stroke".
Endocarditis
Endocarditis is an infection of the inner lining of your heart (endocardium). Endocarditis typically occurs when bacteria or other germs from another part of your body, such as your mouth, spread through your bloodstream and attach to the damaged areas in your heart. Dental procedures can predispose to endocarditis, if proper precautions and pre procedural medications are not well taken care of.
Oral Health and Diabetes
Diabetes mellitus is a metabolic disorder characterized by hyperglycaemia (elevated blood sugar levels) due to the defective secretion or activity of insulin, the hormone that converts sugar into energy.
The working relationship between diabetes and periodontitis may be the strongest of all the connections between the mouth and body. Inflammation that starts in the mouth seems to weaken the body’s ability to control blood sugar.
Studies demonstrate that periodontal disease (advanced form of gum disease), further complicates diabetes because the inflammation impairs the body’s ability to utilize insulin, and so sugar is accumulated in the blood. Moreover, induced production of the body’s own inflammatory mediators to combat periodontal disease also mediates insulin resistance and reduces insulin action.
To further complicate matters, diabetes and periodontitis have a two-way relationship. High blood sugar provides ideal conditions for infection to grow, including gum infections.
A vicious cycle is thus created, where the diseased gum condition negatively affects sugar breakdown, elevating blood sugar levels, increasing susceptibility to infections, impairing tissue repair, increasing gum tissue break down, increasing inflammation, impairing insulin function, increasing blood sugar content and so on.
Accordingly, one should understand that if one has gum disease, then he/she is susceptible to have an increase in his/her blood glucose levels and should try to control it at least partially by managing gum disease by a periodontist (gum therapy specialist).
Fortunately you can use the gum disease-diabetes relationship to your favor: Managing one can help bring the other under control.
Medical treatment using medications is not the only way to control diabetes. Professional dental care to eliminate possible pathways of blood glucose elevation should be an essential part of managing patients with diabetes.
Oral Health, Pregnancy and your Baby
Babies born too early or with a low birth weight often have significant health problems, including lung conditions, heart conditions, and learning disorders. While many factors can contribute to premature (early) or low birth weight deliveries, researchers are looking at the possible role of gum disease. Infection and inflammation in general seem to interfere with a baby’s development in the mother’s womb.
Preterm low-birth weight, as defined by the 29th World Health assembly in 1976, is a birth weight of less than 2500 grams with pregnancy duration of less than 37 weeks.
Preterm and /or low birth weight continues to be a significant cause of infant disease and infant death (morbidity and mortality). This is associated with risk for baby’s death in the first year of life, with developmental problems in childhood, and with risk of several diseases in adulthood. According to various studies, the prevalence of preterm birth varies from 6% to 15% of all deliveries.
The placental complex (which is the temporary organ that joins the mother and fetus, transferring oxygen and nutrients from the mother to the fetus and permitting the release of carbon dioxide and waste products from the fetus) may be affected by infections located far away from it.
This may be due to an indirect action of the movement of bacterial products from one place to another (translocation) such as lipopolysaccharides (which are a major component of some bacterial cell walls that trigger immune response and inflammation) and/or the action of maternally induced inflammatory mediators that may adversely affect pregnancy outcomes.
Bacteria associated with advanced gum disease, may cause inflammation of the placental membrane. Bacterial lipopolysaccharide triggers release of a variety of biologically active mediators (eg: interleukin Ibeta , tumor necrosis factor-alpha & prostaglandin E2). These locally (i.e. orally) produced mediators are released by the body to fight and control the advanced gum disease. On the other hand, they may have a systemic effect, which may contribute to premature labour. Studies have also shown that these advanced gum infections may also impair fetal growth and trigger increased levels of biological fluids that induce preterm labour.
Hence, periodontal (advanced gum disease) has the potential to influence preterm low birth weight through an indirect mechanism involving inflammatory mediators or a direct bacterial assault on the amnion, which is the sac that encloses the developing fetus (baby).
Therefore, gum disease might be a newly considered risk factor of adverse pregnancy. Studies showed that preterm deliveries were 7.5-fold more common in women with severe gum disease than in those with good gum health. Studies have also shown that women whose periodontal condition (meaning the soft and hard tissues surrounding the teeth) worsens during pregnancy have an even higher risk of having a premature baby.
It is therefore highly advised to have a thorough clinical and radiographic full mouth assessment before thinking of becoming a mom. For the best chance of a healthy pregnancy, and a healthy to be baby, please visit a specialized gum therapist. You will improve your oral health and protect your general and baby’s health.
Your Breathing System
There are many diseases that affect the breathing system especially the lungs. Among the serious conditions, are the pneumonias, which are a group of diseases caused by a wide variety of infectious agents, including bacteria, fungi, parasites, and viruses, resulting in infection of the lung organ responsible for gas transfer (parenchyma). Pneumonia can be a life-threatening infection, especially in the elderly and patients with suppressed/depressed immunity (i.e. reduced ability to fight against infections and protect own body).
Other respiratory diseases also include chronic bronchitis (which is an inflammatory condition associated with excessive mucous production) and emphysema (which is the destruction of the air spaces with destruction of the alveolar septa). These conditions whether separate or collectively may lead to chronic obstructive pulmonary disease characterized by chronic obstruction to airflow making breathing difficult.
It is possible that aspiration of (oral) bacteria may worsen the course of chronic obstructive pulmonary disease. It is also known that one of the most common routes of infection for bacterial pneumonia is aspiration of oral and throat contents. Bacteria that grow in the mouth and throat can be aspirated into the lower respiratory tract and lungs to contribute to respiratory diseases such as pneumonia or worsening lung conditions. Studies have also demonstrated that recurrent respiratory diseases and/or tonsillitis conditions may be related to the translocation of bacterial reservoir at areas of partially impacted wisdom teeth.
The possibility that bacteria in oral plaque influence respiratory infection suggests that good personal and professional (in dental office) oral hygiene may prevent the aspiration of large numbers of oral bacteria into the lower airway and thus prevent initiation or progression of respiratory infection in susceptible individuals.
Oral Health and Osteoporosis
Osteoporosis and advanced gum disease (periodontitis) have an important thing in common, bone loss. The link between the two, however, is controversial. Osteoporosis affects the long bones in the arms and legs, whereas gum disease/periodontitis attacks the jawbone. Others point to the fact that osteoporosis mainly affects women, whereas periodontitis is more common among men.
Though a link has not been well established, some studies have found that women with osteoporosis have gum disease more often than those who do not. Researchers are testing the theory that inflammation triggered by periodontitis could weaken bone in other parts of the body.
Rheumatoid Arthritis
Obesity
Oral and maxillofacial surgeons are dentists specialized in surgery of the mouth, face and jaws. After four years of dental school, surgeons receive four to seven years of hospital-based surgical and medical training, preparing them to do a wide range of procedures including all types of surgery of both the bones and soft tissues of the face, mouth and neck.
Periodontists are dentists who specialized in the diagnosis and treatment of periodontal (gum) disease. They have had extensive training with two to three additional years of study after dental school. As specialists they devote their time, energy and skill to helping patients care for their gums which has a direct effect on their general health. Periodontists are generally recognized as good dental implantologists. They take good care of all the tissues surrounding the teeth and dental implants which affects the health and longevity of these elements. A periodontist is one of the eight dental specialists recognized by the American Dental Association.
The Endodontist examines, diagnoses and treats diseases and destructive processes, including injuries and abnormalities of dental pulps (nerves) and underlying tissues of the teeth.
Endodontists examine patients and interpret radiographs and nerve tests to determine pulp vitality and periapical tissue condition. They evaluate their findings and prescribe a method of treatment to prevent loss of teeth.
A pediatric dentist has at least two additional years of training beyond dental school. The additional training focuses on management and treatment of a child’s developing teeth, child behavior, physical growth and development, and the special needs of children’s dentistry. Although either type of dentist is capable of addressing your child’s oral health care needs, a pediatric dentist, his or her staff, and even the office décor are all geared to care for children and to put them at ease. If your child has special needs, care from a pediatric dentist should be considered.
An orthodontist prevents and treats mouth, teeth, and jaw abnormal relations and proportions. Using braces, retainers, and other devices, an orthodontist helps straighten a person’s teeth and correct the way the jaws line up with the face.
Orthodontists treat kids and adults for many problems, including having crowded or overlapping teeth or having problems with jaw growth and tooth development. These tooth and jaw problems may be caused by tooth decay, losing baby teeth too soon, accidents, habits like thumb sucking and even gum diseases. These problems can also be genetic or inherited.
Good oral hygiene is important, not only for looks, but for general health as well. Poor oral hygiene can lead to a variety of dental and medical problems such as gum disease, infection, bone loss, heart disease, strokes and more. Regular check ups and cleanings can prevent these problems as well as provide you with good oral hygiene.
1. To Prevent Oral Cancer
According to The Oral Cancer Foundation, someone dies from oral cancer, every hour of every day in the United States alone. When you have your dental cleaning, your dentist is also screening you for oral cancer, which is highly curable if diagnosed early.
2. To Prevent Gum Disease
Gum disease is an infection in the gum tissues and bone that keep your teeth in place and is one of the leading causes of adult tooth loss. If diagnosed early, it can be treated and reversed. If treatment is not received, a more serious and advanced stage of gum disease may follow. Regular dental cleanings and check ups, flossing daily and brushing twice a day are key factors in preventing gum disease.
3. To Help Maintain Good Physical Health
Recent studies have linked heart attacks and strokes to gum disease, resulting from poor oral hygiene. A dental cleaning every 6 months helps to keep your teeth and gums healthy and could possibly reduce your risk of heart disease and strokes.
4. To Keep Your Teeth
Since gum disease is one of the leading causes of tooth loss in adults, regular dental check ups and cleanings,brushing and flossing are vital to keeping as many teeth as you can. Keeping your teeth means better chewing function and ultimately, better health.
5. To Detect Dental Problems Early
Your dentist and hygienist will be able to detect any early signs of problems with your teeth or gums. Early detection of cavities, broken fillings and gum disease are easily treatable. If these problems go untreated, root canals, gum surgery and removal of teeth could become the only treatment options available.
6. To Maintain Good Oral Health
Your dental hygienist will help to ensure that you are maintaining your good oral health by visual examination and comparing your previous dental check ups. If you are falling off track with your oral hygiene he / she will help put you back on the right path.
7. To Use Your Dental Insurance Plan
Dental insurance plans usually pay for all or most of the cost of dental cleanings and check ups every six months. Take advantage of this and save a lot of money in the long run by avoiding costly dental procedures that can result from poor oral hygiene.
8. To Create a Treatment Plan
If your dentist diagnoses any problems in your mouth, he /she will most likely give you a treatment plan. This treatment plan should have the cost of each procedure that you will need, so that you can discuss financial arrangements with the front office.
9. To Have a Bright and White Smile
Your dental hygienist can remove most tobacco, coffee and tea stains. During your cleaning, your hygienist will also polish your teeth to a beautiful shine. The result? A whiter and brighter smile!
10. To Prevent Bad Breath
Dental studies show that about 85 percent of people with persistent bad breath, also known as halitosis have a dental problem that is to blame. Good oral hygiene is essential in preventing bad breath. Regular check ups and cleanings are the best way to make sure that you are maintaining good oral hygiene.